7 Ultimate Steps to Conquer Fungal Acne For Good

|
Getting your Trinity Audio player ready...
|
Dealing with stubborn, itchy bumps that refuse to go away can be incredibly frustrating, especially when your usual acne treatments don’t work. You might be surprised to learn that what you believe is traditional acne could actually be something different entirely. This condition, known as fungal acne, requires a unique approach to treatment and care. Understanding its specific causes and symptoms is the first crucial step toward achieving clear, healthy skin.
This guide will provide a comprehensive look at fungal acne, from its scientific name, Malassezia folliculitis, to its distinct characteristics. We will explore what causes this common skin issue and how it differs from bacterial acne. You will learn about effective treatment options, lifestyle changes, and preventative measures to manage outbreaks. By the end, you’ll have the knowledge and tools to identify and effectively conquer fungal acne.
What Exactly Is Fungal Acne?
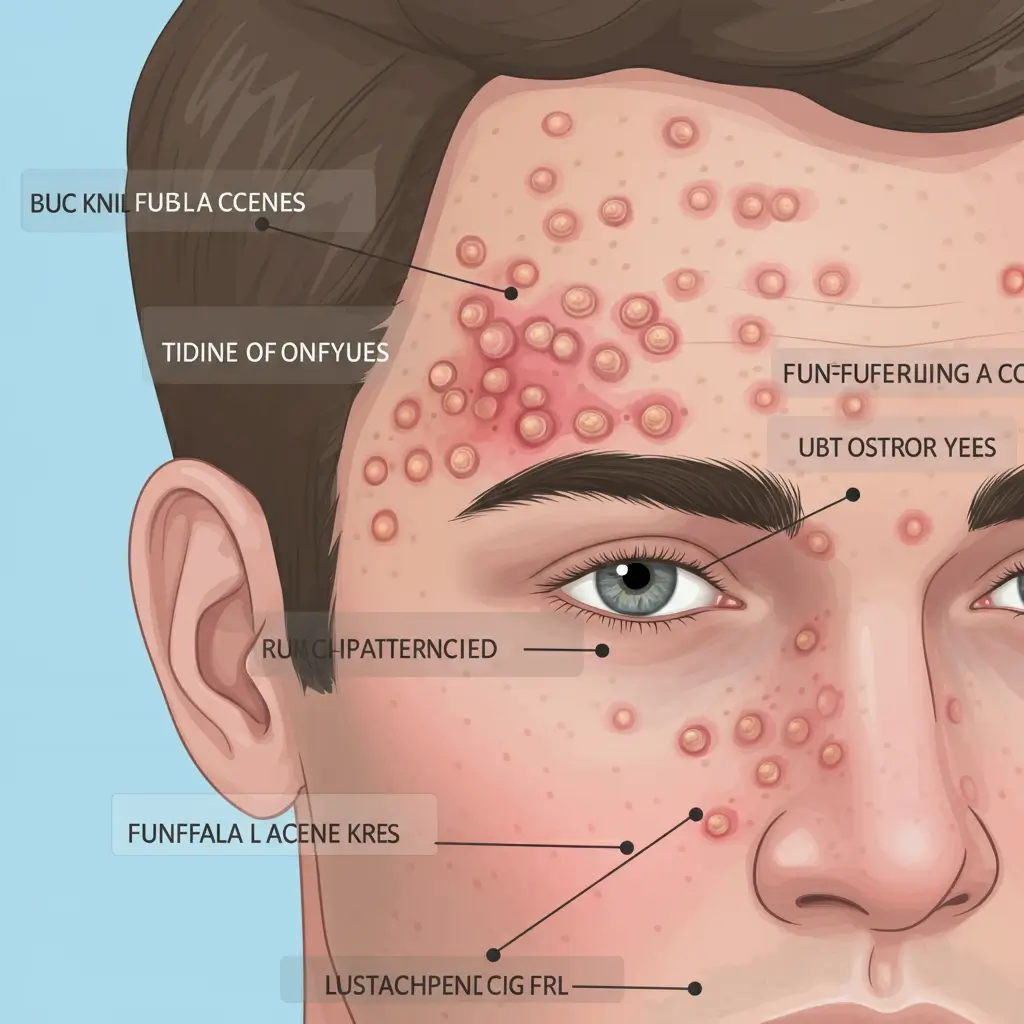
Fungal acne, or Pityrosporum folliculitis or Malassezia folliculitis, is an infection of the hair follicles on your skin. Despite its name, it isn’t true acne in the traditional sense. It’s caused by an overgrowth of yeast, a type of fungus called Malassezia, which is naturally present on everyone’s skin. Normally, this yeast coexists peacefully with other microorganisms, but certain conditions can cause it to multiply excessively, leading to inflammation and acne-like eruptions.
These breakouts typically appear as small, uniform, itchy pustules or papules. They often show up in clusters on the chest, back, upper arms, and sometimes the face, particularly along the hairline and forehead. Because it thrives in moist environments, fungal acne is more common in people who live in hot, humid climates or who sweat frequently. Unlike bacterial acne, these bumps are often very itchy and can be persistent if not treated correctly.
Fungal Acne vs. Bacterial Acne: How to Tell the Difference
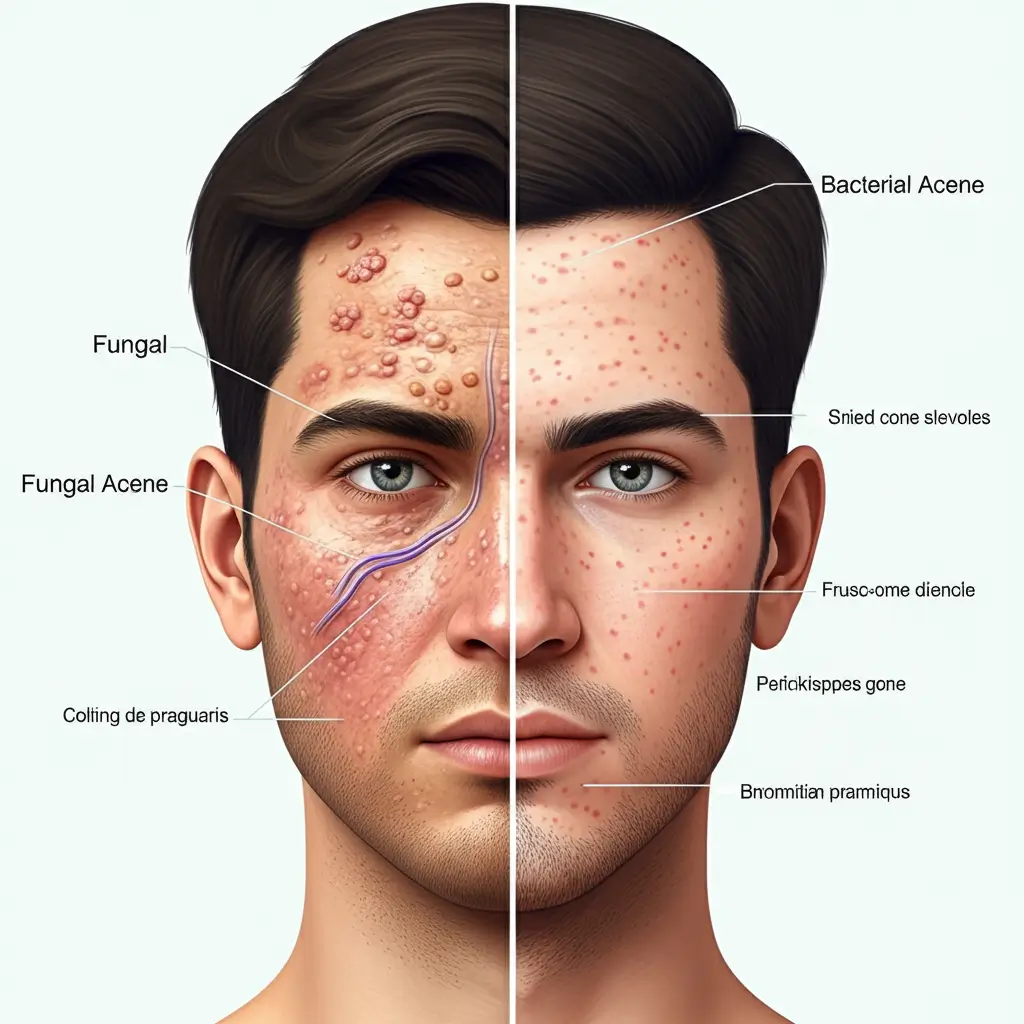
Distinguishing between fungal acne and bacterial acne (acne vulgaris) is vital because they require different treatments. Using traditional acne products on fungal acne can sometimes make the condition worse. The most significant difference lies in the appearance and symptoms of the breakouts. Fungal acne lesions are typically monomorphic, meaning they are all roughly the same size and shape—usually small, red bumps or whiteheads around 1-2 millimeters in diameter.
Bacterial acne, on the other hand, presents with a variety of lesion types, including blackheads, whiteheads, papules, pustules, nodules, and cysts of different sizes. Another key differentiator is the sensation. Fungal acne is almost always accompanied by significant itching, a symptom not commonly associated with bacterial acne. If your “acne” is very itchy and consists of uniform bumps, there’s a good chance you are dealing with a fungal issue. A dermatologist can confirm the diagnosis by examining a skin scraping under a microscope.
Key Causes of Fungal Acne Outbreaks

An overgrowth of Malassezia yeast is the direct cause of fungal acne, but several factors can trigger this imbalance. Understanding these triggers is essential for both treatment and prevention. One of the primary culprits is excessive moisture and sweat. Wearing tight, non-breathable clothing, especially during exercise, traps sweat and heat against the skin, creating the perfect warm, humid environment for yeast to flourish.
Certain lifestyle and health factors also play a role. A weakened immune system, whether due to illness or medications like corticosteroids, can disrupt the skin’s natural balance. The use of antibiotics is another common trigger; these medications reduce the bacteria on your skin, which can allow the Malassezia yeast to grow unchecked. Furthermore, a diet high in sugar and carbohydrates may contribute to yeast overgrowth throughout the body, including on the skin.
Effective Treatments to Clear Fungal Acne

Since fungal acne is a yeast infection, it requires antifungal treatments rather than the benzoyl peroxide or salicylic acid used for bacterial acne. Your approach can include both over-the-counter (OTC) options and prescription medications, depending on the severity of the outbreak.
Over-the-Counter Solutions
For mild cases, you can start with topical antifungal products. Many people find success using anti-dandruff shampoos as a body or face wash. Look for shampoos containing active ingredients like ketoconazole (found in Nizoral) or selenium sulfide (found in Selsun Blue). To use this method, apply the shampoo to the affected areas, let it sit for five to ten minutes to allow the active ingredient to work, and then rinse it off thoroughly. Do this daily for a week, then reduce the frequency to a few times a week for maintenance.
Prescription-Strength Options
If OTC treatments don’t resolve the issue, it’s time to see a dermatologist. They can prescribe stronger topical antifungal creams or lotions containing higher concentrations of ketoconazole, econazole, or clotrimazole. For widespread or persistent cases of fungal acne, your doctor might recommend oral antifungal medications. Pills like fluconazole or itraconazole are highly effective at clearing the infection from the inside out. These are typically prescribed for a short course to bring the yeast population back under control.
Building a Fungal Acne-Safe Skincare Routine
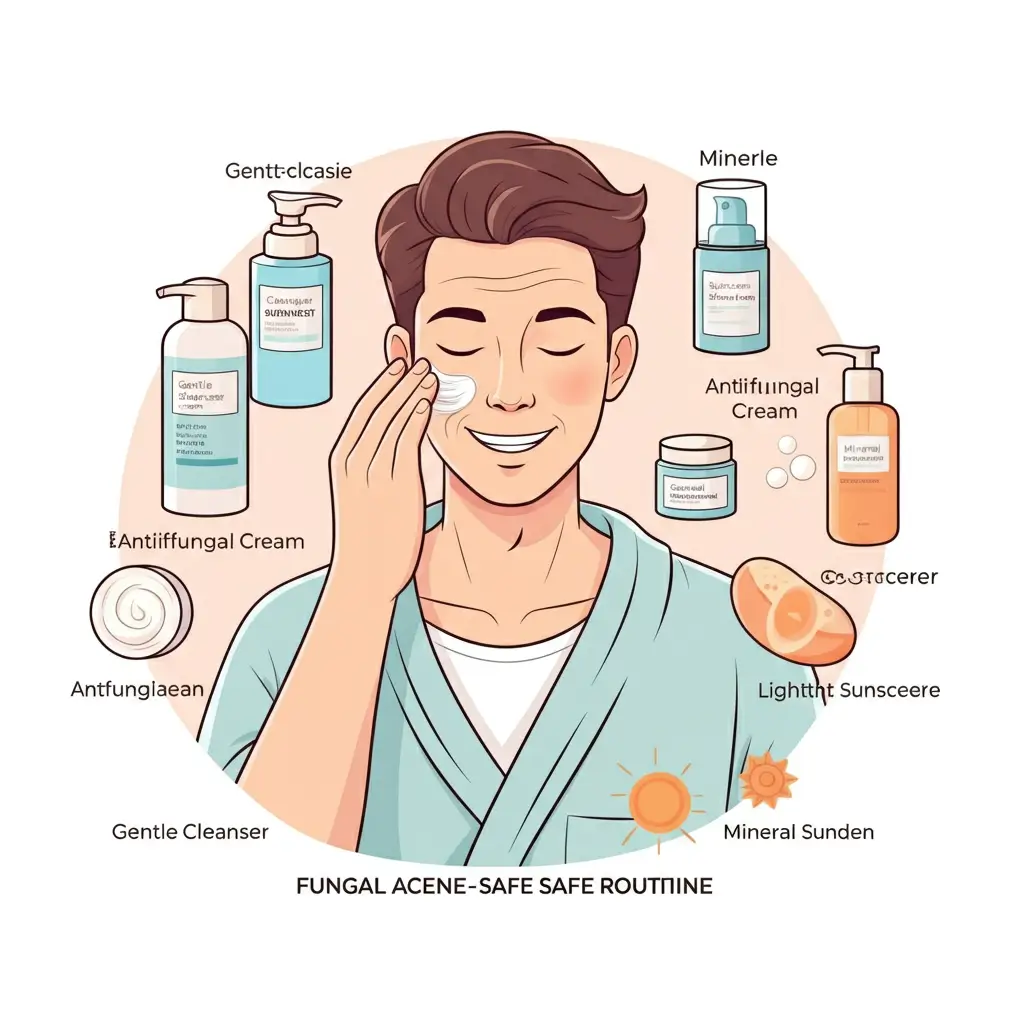
Adjusting your skincare routine is crucial for managing and preventing fungal acne. The goal is to avoid ingredients that can feed the Malassezia yeast. This means you’ll need to become an expert at reading ingredient labels. Many common skincare ingredients, particularly certain oils, fatty acids, and esters, can exacerbate fungal acne. A good rule of thumb is to look for products labeled as “fungal acne-safe.”
A simple, effective routine might look like this:
- Cleanse: Use a gentle, fungal acne-safe cleanser. If you are actively treating a breakout, you can use an antifungal shampoo as your cleanser for a short period.
- Treat: Apply any prescribed topical antifungal creams as directed by your dermatologist.
- Hydrate: Moisturizing is still important. Opt for a lightweight, oil-free, and fungal acne-safe moisturizer. Ingredients like squalane (derived from sugarcane, not olives), glycerin, and hyaluronic acid are generally safe choices.
- Protect: Sunscreen is a must. Choose a mineral-based, oil-free formula to protect your skin without clogging pores or feeding the yeast.
Lifestyle and Diet Changes for Prevention
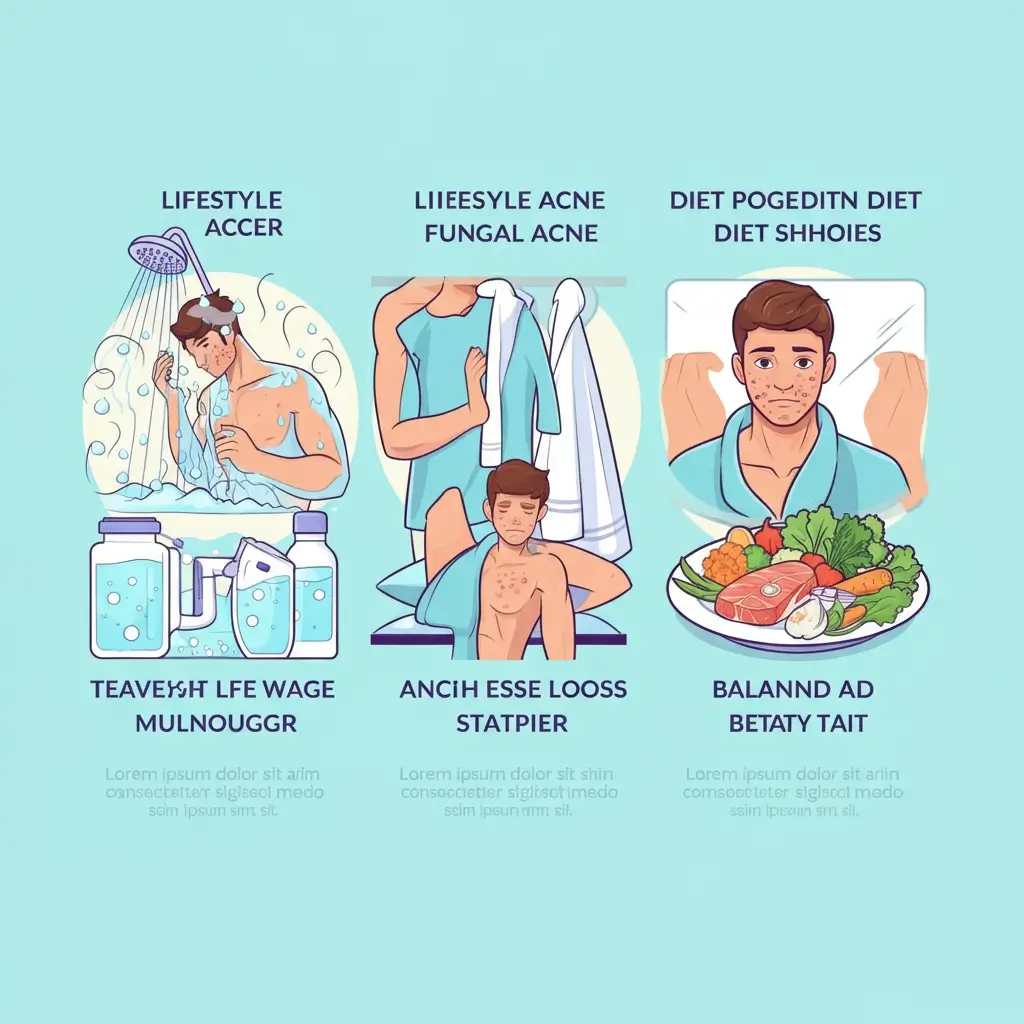
Beyond skincare, certain lifestyle adjustments can make a big difference in preventing future fungal acne flare-ups. Since yeast thrives in damp environments, one of the most impactful changes you can make is to manage sweat. Shower immediately after working out or any activity that causes you to sweat heavily. Change out of sweaty clothes as soon as possible.
Wearing loose-fitting, breathable fabrics like cotton or linen can also help reduce the buildup of heat and moisture against your skin. Pay attention to your diet as well. While the link is still being studied, some evidence suggests that limiting your intake of sugar and refined carbohydrates may help control yeast growth. Focusing on a balanced diet rich in vegetables, lean proteins, and whole grains supports overall skin health and may help keep fungal acne at bay.
Frequently Asked Questions (FAQs)
1. How long does it take for fungal acne to go away?
With proper antifungal treatment, you can often see improvement within a few weeks. However, it may take one to two months for a breakout to clear completely.
2. Can I use benzoyl peroxide on fungal acne?
It’s not recommended. Benzoyl peroxide targets bacteria, not fungus, and it can dry out and irritate the skin, potentially making the condition worse.
3. Is fungal acne contagious?
No, fungal acne is not contagious. The Malassezia yeast that causes it is a normal part of everyone’s skin flora. The condition only occurs when there is an overgrowth of this yeast.
4. Does diet really affect fungal acne?
While research is ongoing, some anecdotal evidence suggests that diets high in sugar and carbohydrates can promote yeast growth. A balanced, low-sugar diet may help some individuals manage their symptoms.
5. How do I know if my skincare products are fungal acne-safe?
You can check the ingredient list of your products against online databases that identify ingredients known to trigger fungal acne. Look for oil-free formulas and avoid most fatty acids and esters.
Conclusion
Successfully treating fungal acne involves correctly identifying the condition and adopting a targeted approach to care. Unlike traditional acne, this yeast-driven issue requires specific antifungal treatments and careful attention to your skincare ingredients. By using products like ketoconazole shampoo and avoiding oils and fatty acids that feed Malassezia, you can effectively clear active breakouts. Remember that consistency is key to seeing results and restoring balance to your skin’s microbiome.
Beyond immediate treatment, long-term prevention is centered on creating an environment where yeast cannot thrive. This includes making simple lifestyle changes such as showering after exercise and wearing breathable clothing. Pairing these habits with a fungal acne-safe skincare routine and a balanced diet will help you maintain clear skin. With the right knowledge and strategy, you can confidently manage Malassezia folliculitis and prevent it from returning.






